As she rushes to her gate, the traveller can see her plane through the airport window, sitting on the tarmac, loaded and ready to leave.
After a year of drastically reduced travel, the airport is bustling. As she approaches the desk, she pulls out her usual passport and boarding pass, then opens a new app.
She shows it to the boarding agent, and it flashes her confirmation: She has the required vaccine.

It’s the kind of scene that’s becoming increasingly easy to imagine as a working COVID-19 vaccine gets closer to regulatory approval.
Suddenly, things such as travel passes that vouch for your vaccination status, concerts that require a shot to get in the door, or even questions about whether business might refuse to serve the unvaccinated are no longer the purview of speculative fiction writers, but of policymakers, experts and members of the general public.
With doses expected to be scarce, at least at first, we appear set to enter a new era of uneven vaccine access, beginning the day the first doses become available, and ending when they become available to everyone.
That time in the middle? Likely to stretch at least a year in Canada, it will force us to confront questions about who gets a vaccine, when to keep track and how we might take our first tentative steps back to normalcy.
It could also, experts warn, give rise to inequities as the vaccine splinters society into the haves and the have nots.
“I keep thinking about that Dr. Seuss book about the star-bellied Sneetches,” says Alison Thompson, an associate professor in the faculty of pharmacy at the University of Toronto, who specializes in public health ethics.
“They’re basically these little birdlike creatures, and some of them have stars on their bellies, and some don’t,” she says.
In the book, the Sneetches with stars discriminate against those without despite the fact the stars are largely out of their owners’ control.
Thompson raises the question: Could vaccines play out in the same way?
“You know, while it may not be something that’s visible on our skin, it’s certainly something that can be used to mark us as different from one another.”
When the first vaccine is rolled out
Speaking to reporters who were either masked or watching via livefeed, as has become the new press conference norm, said last week that a vaccine could land as early as the first months of next year.
It’s a light at the end of the tunnel that has only burned brighter since have rolled in from several leading vaccine candidates.
Once approved by Health Canada, the first vaccine doses are expected to be in short supply, initially. With that in mind, the National Advisory Committee on Vaccines has released recommendations on who it thinks should be first in line.
In order to “minimize serious illness and overall deaths while minimizing societal disruption as a result of the COVID-19 pandemic,” the group argues it should be those at high risk of serious illness or death, those who are likely to transmit it to those at high risk, and essential workers.
In other words, if you’re young and healthy, you may have to wait.
But even once you get a shot, don’t expect it to be a magic bullet, says Dr. Prabhat Jha, an epidemiologist and professor of global health at the University of Toronto.
“If you got vaccinated tomorrow or I got vaccinated tomorrow, it doesn’t mean we go out on the street and kiss people,” he said. “The face masks and physically distancing will have to continue.”
In the short term, a vaccine will reduce your chance of getting COVID-19, but it’s not clear yet how effective the vaccines will be in stopping transmission.
So it’s possible that you could still be carrying the virus and giving it to others. It will take time for the country to reach what’s called herd immunity, when enough people are either immunized or have recovered from COVID-19 that spread slows.
Once people are vaccinated, it’ll become slightly easier to go out to eat or see friends, Jha says, but a vaccine won’t undo the past year.
“We have to be realistic,” he said. “Hopefully, it means a lot more normalcy in terms of how we can carry on, but all these things that we’re doing now? In most part, they would need to continue.”
Tracking who is vaccinated, and who is not
Half a world away, a pilot project is rolling out in eastern Africa that might provide a model for our post-vaccine world.
There are truck drivers who regularly pick up loads of food and essential supplies in port cities in Kenya or Tanzania, then set out for the cluster of landlocked countries just inland, knitted to the coast only by road.
When they approach a border, they pull out a phone and show the screen to an official to verify that they’ve recently tested negative for COVID-19, using a test and within a time frame that has been agreed to by all countries in advance.
This process is in place among a group of six countries known as the East African Community, which often work together as a single economic bloc.
Together, the countries asked a Swiss-based non-profit public trust, The Commons Project, to create a technology platform that would certify that drivers had taken a recent, credible COVID-19 test and weren’t carrying the pandemic across borders.
There is precedent for the approach. Cards certifying the carrier has been vaccinated for yellow fever have long been common in parts of Africa and South America.
The fast-changing nature of COVID-19, though, demands a digital approach, says The Commons Project’s chief medical officer, Dr. Brad Perkins.
A digital platform is able to keep pace; putting it on a phone means it can be easily verified, he says. “It’s not simple, but it’s doable.”
Now, the project is hoping to take the lessons learned in East Africa and apply it to the world, with the creation of a new platform called CommonPass, which, the project hopes, will allow anyone on the planet to eventually certify their testing or vaccination status.
The project recently tested the prototype on flights with two different airlines, one from Hong Kong to Singapore and the other from London to New York, with the aim of having a working version ready by early next year.
CommonPass doesn’t try to make claims about anyone’s immunity. Instead, it’s like carrying around your testing or vaccination history in your pocket, Perkins says.
The promise of the technology comes with a spectre of concern for some.
“For the safety of patients, it’s important to know who has and has not received a vaccine, despite concerns about having that information being tracked in any way,” says Maxwell Smith, a public health ethicist at Western University who is a member of the World Health Organization’s ethics and COVID-19 working group.
“But there’s a separate issue of what we do with that information, and whether that creates a system that would prevent some people from working or from going to school or travelling or whatever it might be used for.
“And I think that’s where we get into a very ethically murky territory.”
But Perkins, who previously worked in public health for the American Centre for Disease Control, said the team behind CommonPass is sensitive to the “slippery ethical slope” here.
Countries will get to decide what their specific entrance requirements are — perhaps they want travellers to have had a certain vaccine, or have had it within a certain time period. All CommonPass is doing is verifying whether a person has met that requirement. The pass does not share anyone’s health data with governments or airlines, he adds.
Travel will be never be totally risk free, he says, but the goal is to make it possible for people to control their own health data and countries, . There will be a printable version for people who don’t have phones. The non-profit hopes to make the platform free to travellers, but charge airlines a fee to pay for the infrastructure.
“There’s lots of hand waving about apps and mobile devices and technology,” he says. “All it boils down to is: Countries have an urgent need to find a way to trust a laboratory result or, in the case of vaccines, vaccination status, that originated in another country.
“This is all about creating global trust in the ability to share high-quality health data that can make international travel safer.”
Canada vs. The World
The problem of a class system divided by vaccine — “vaccinated versus unvaccinated” — is also poised to go global.
It seems likely that Canada will be able to vaccinate its population before many countries around the world.
What then?
Would Canada close its borders to the unvaccinated? Should Canadians be allowed to go abroad while the pandemic still rages elsewhere?
Smith says we may see rich countries opening back up and starting to travel and trade with each other long before poorer countries, which will only widen the divide between rich and poor globally.
He adds that the virus doesn’t recognize borders, so it’s arguably in Canada’s interest to help other countries.
“If Canada can play a role in ensuring that other countries are getting the vaccine that they need as well, that isn’t just a function of charity, it’s actually helping to protect our interests as well.”
‘A splintering in society’
Here at home, there will also likely be pressure to keep track of who is vaccinated and who is not.
BBC reported that Ticketmaster has been exploring some sort of vaccine policy for concertgoers, although the company was adamant it will not require vaccines.
This summer, USA Today from three professors from Case Western Reserve University in Ohio in which they argued those who don’t take a vaccine should be denied non-essential government services and face higher insurance premiums. They said businesses should be allowed to refuse to both employ and serve the unvaccinated.
Thompson says these scenarios, where an employer wants staff back at work, but demands vaccination status, or insurance companies that jack up premiums for those who don’t line up for the shot, are real concerns.
“Do we need a sort of moratorium on hiring and firing based on immune status? It’s not easy, though, because there are some places that justifiably require that, like health-care institutions, for example. So it can’t be a blunt instrument.”
While it’s not a completely unreasonable idea, Smith said, he remains wary of any commercial entity that would require vaccination status. “It really seems like we’re scrambling to identify anything that will allow us to get back to normal,” he says.
“If by simply having that as a checkbox, that means we can have big concerts or have big sporting events again? Then I think there’s a sort of an undue influence for commercial entities to do that, no matter whether it’s responsible or ethically appropriate.”
From a business perspective, he argues, there won’t be enough vaccinated people at first to justify running a concert or sports game just for them. Later on, the hope is that herd immunity will start to kick in, so there’ll be less justification for keeping the unvaccinated out.
“I also think that it creates a splintering in society of those who are able to access a vaccine,” he adds. “That’s going to put some in a more advantageous position if they’re able to go to concerts or go to school or go to work or whatever the vaccination status would sort of allow you to do.
“I think that’s something we need to be really careful about doing.”
Smallpox and history’s lessons
Canada’s early history is punctuated by resurgences of and battles against the so-called “speckled monster.” As deadly as Ebola, smallpox wiped out whole towns, was occasionally debated as a weapon and killed untold thousands.
When a came to Quebec in 1769, just a handful of years after it fell to the British, that protection came first to the well-to-do families in Montreal and Quebec City, and to the British troops stationed nearby.
Priorities haven’t shifted a huge amount since then, either. Almost two and half centuries later, players for the Calgary Flames were able to skip the line to get the H1N1 vaccine in 2009 — though it did spark outrage among the general public.
Assuming we choose to follow the prevailing advice to vaccinate the most vulnerable first, there will still come a day when seniors and health-care workers are protected, and we’ll have to decide who comes next.
That decision may get harder.
It will be important, Thompson says, that the government is clear about who is vaccinated and why. People should have a chance to voice their opinions about who should be prioritized.
“Science alone isn’t going to tell us what to do here,” she said. In many ways, questions about who to vaccinate reflect what we value as a society. Who do we want to protect most? Is businesses opening first the most important thing?
“These are value judgments and society ought to weigh in on these kinds of questions.”
Of course, regardless of who is vaccinated first, once those doses start rolling out, a divide may begin to emerge.
“We’ve been, to some extent, all in it together up until this point; but once people start getting vaccinated, it becomes vaccinated versus unvaccinated,” Thompson said.
Once people get vaccinated, you might see them become less willing to follow public health orders or to engage in the sort of social distancing and mask wearing that would protect the unvaccinated, Smith adds.
Remember, just because you’re vaccinated doesn’t mean you’re infallible — or that you can’t spread the virus. (The new vaccines might help with transmission, but that remains to be seen.)
“If 10 per cent of our population were to become vaccinated, and if we can imagine that the vaccine were something like 90 per cent effective, having those 10 per cent of people travelling all around Canada, or travelling all around the world, and not adhering to other public health measures that we have in place, could be detrimental to the rest of the population,” he said.
Many experts worry about the number of people who will choose to reject the shot.
Revisiting the history of smallpox again shows this is not a new issue.
were more skeptical than their northern neighbours from the start about new concepts such as vaccination, or its crude predeccsor, known as variolation, because of religious concerns it interfered with God’s domain. It has even been argued that differing rates of immunization played a role in the American Revolution and General George Washington’s failed invasion.
When Washington launched his attack in 1775, his forces were quickly laid low by a smallpox outbreak that largely bounced off the immunized British forces north of the St. Lawrence River.
Washington’s troops retreated, and what would become Canada remained part of the British Empire.
Mission accomplished
Many of the decisions about who to vaccinate, and how and why, are being made right now.
Many eyes will be watching to see how this plays out.
“The vaccine has so much riding on it because it’s been held up as the only way out; so we’re starting to think about the end of this pandemic,” Thompson said.
“But what do we want society to look like on the other side of all this? What kind of damage is going to be done by not getting this right, by not engaging with the people, by not building those trusting relationships between the citizenry and public health and government?
Smith points to how the pandemic has cracked the inequalities in our society wide open.
The pandemic has not hit us all equally, and we don’t all have the same access to health care. Maybe, he said, the vaccination campaign will be another chance to rebalance the scales.
“It’d be great if we could really appreciate the lessons from what we’ve seen for the past 10 months.”










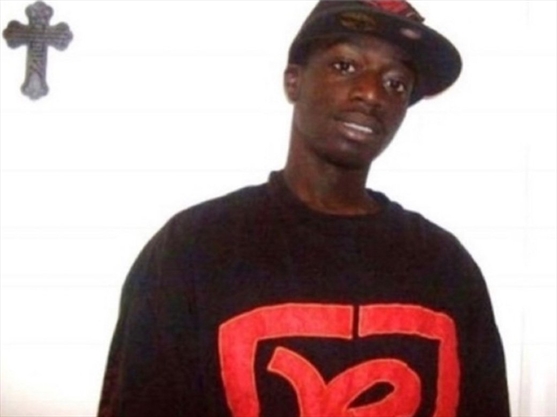

 Brothers Prince Appiah, left, and Junior have their photo taken around Christmas time years ago. – Appiah family photo
Brothers Prince Appiah, left, and Junior have their photo taken around Christmas time years ago. – Appiah family photo









