‘Ontario is at a breaking point:’ COVID-19 impacts being felt beyond the lockdown areas of Toronto and Peel
The impacts of are radiating out further from the lockdown zones of Toronto and Peel as the province marked a sixth straight day with new cases above 1,700 and 35 deaths, the highest in a week.
Hospitals in Kitchener, Cambridge and Windsor are among those feeling the pinch of a growing pandemic that has already curbed non-emergency surgeries in parts of the GTA.
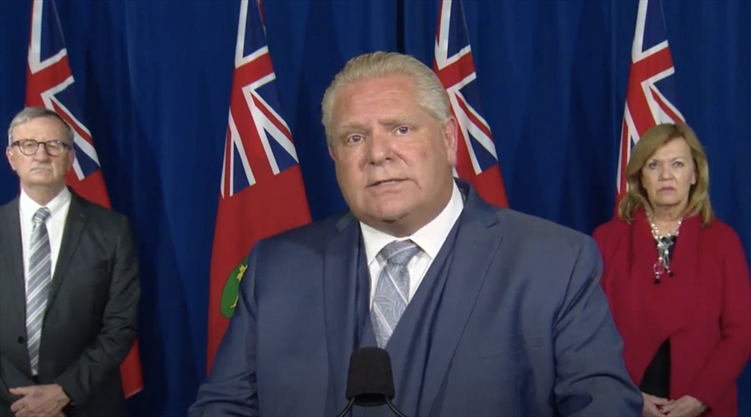
Health Minister Christine Elliott said parts of the province could see more restrictions imposed on them Friday after the latest statistics are re-evaluated by Ontario’s chief medical officer Dr. David Williams.

“Dr. Williams is speaking with the medical officers of health in several other areas to obtain their views about whether…they think they should be moved up from orange to red or into lockdown,” she told reporters Wednesday in a reference to the province’s five-tier, colour-coded framework.
Criteria include the weekly rate of cases per 100,000 people, the number of outbreaks, strain on hospital intensive care unit capacity and the percentage of people testing positive, along with a health unit’s ability to keep up with contact tracing.
York Region, Durham, Halton, Hamilton, Waterloo and Windsor-Essex are now in the red zone, one step short of lockdown.
In Kitchener, Grand River Hospital said it has temporarily paused non-urgent elective surgeries and has cut down to two cardiac surgeries a week.
“We are currently at full capacity in ICU (intensive care unit) and are experiencing a surge in COVID and non-COVID critical-care patients,” the hospital said in a statement as the surrounding Waterloo public health unit reported 103 new infections.
Waterloo MPP Catherine Fife called on Premier government to provide “immediate and urgent investments” for hospitals.
“Ontario is at a breaking point…things are only going to get worse,” the New Democrat said in the legislature’s daily question period.
Elliott maintained “Ontario is not in a crisis right now” and said it is doing better than Alberta and Manitoba which have case rates four and six times higher, with Alberta “doubling up” patients in intensive care rooms.
“We are flattening this curve,” Elliott said.
Figures from her own ministry show active cases are at an all-time high of 14,526 people testing positive in the last 14 days and the seven-day average of cases hitting a record of 1,720, up 50 people from Tuesday.
There were 1,723 new cases reported Wednesday, up slightly from 1,707 the previous day.
Elliott later acknowledged Ontario has “plateaued at a very high level but what we want to do is keep it there, but move it down.”
She came under fire from opposition parties for comparing Ontario to worse-off provinces out west instead of better-off Atlantic Provinces where cases are low because of a restrictive bubble formed there earlier this year.
“Stop playing defence,” said Liberal House Leader John Fraser. “It’s not a valid argument. We need to be better able to manage this.”
The health unit in Windsor-Essex, which had another 60 cases and entered the red or “control” zone on Monday, said it is having trouble keeping up and is battling 18 outbreaks, including two of Ontario’s six current school closures. Hospitals have put strict limits on visitors.
“Every outbreak that we report, every case, is a further stretch of our resources,” said chief executive Theresa Marentette, noting that tracing and managing cases is becoming increasingly difficult.
“We need help and we need it now,” added New Democrat MPP Percy Hatfield (Windsor-Tecumseh), warning of a “looming collapse.”
Elliott said she is aware of the “considerable concern regarding public health resources” in Windsor-Essex and has provided 24 more contact tracing staff to help get case growth “more under control.”
“If more resources are needed for that, we will certainly provide them,” she pledged.
Green Leader Mike Schreiner said areas outside Toronto clearly need more help from the province to stem the tide of the pandemic until a vaccine arrives and is widely distributed.
“The virus can get out of control. The government needs to deploy resources immediately to those areas that need them.”
Most cases remain in the GTA, with Toronto at 410 new infections, Peel with 500, York 196, Durham at 124 and Halton with 45. Hamilton had 74.
Ontario has had 3,698 deaths from COVID-19 since the first fatality in March. Almost 120,000 people have tested positive for the virus, which first arrived in the province in January.
Rob Ferguson is a Toronto-based reporter covering Ontario politics for the Star. Follow him on Twitter: